Infants with cows’ milk protein allergy (CMA) show symptoms due to their immune system reacting to proteins within cows’ milk. These proteins are present in milk and other dairy products, standard infant formula feeds and less commonly they can pass to an infant in breast milk.
The prevalence of milk allergy in the U.K. is said to be 2-3% with most presenting in the first year of life.1 Milk allergy can be IgE-antibody mediated, non-IgE mediated or there may be a mixed presentation with both IgE and non-IgE mediated symptoms.2
Symptoms
IgE mediated symptoms usually occur within minutes to two hours of exposure. In non-IgE mediated disease, the immune reaction develops over time and with repeated exposure, giving delayed symptoms, usually two hours to several days later.2
GP’s play an important role in diagnosing and managing cows’ milk allergy in infants.
Learn more about managing CMA in primary care by completing a short RCGP-accredited module.
This article has been funded by Nestle Health Science UK for GP Connect
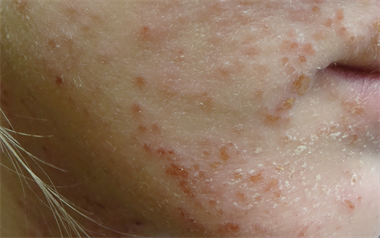
Symptoms of milk allergy are typically in one or more of the gastrointestinal, skin or respiratory systems. IgE mediated disease may present for example with redness and itching around the mouth, urticaria, angioedema, immediate vomiting and rarely anaphylaxis.
The delayed symptoms (non-IgE) include gastro-oesophageal reflux disease, loose, frequent stools or constipation (straining but a soft stool) and atopic eczema. Symptoms in more than one organ system or those not responding to usual management of these symptoms should raise suspicion of CMA.2
Difficulties when diagnosing CMA
One of the difficulties in diagnosing CMA is the array of possible symptoms. Regurgitation, colic and vomiting can all occur in babies with no medical condition and when simple strategies for managing these have proved unsuccessful and symptoms remain troublesome, then CMA may be the cause.2
Determining when to consider a milk exclusion diet, which is the dietary management strategy for both IgE mediated and for non-IgE mediated disease can be difficult.
An allergy-focused history should be taken whenever a food allergy is suspected.2,3 There are usually clues within the history, which suggest CMA should be considered e.g. a family history of asthma, eczema or a food allergy.
Although the diagnosis cannot be ruled out if there is no atopic family history, it is more likely.2 It is also worth considering when there is a family member with a label of 'lactose intolerance', which presented in infancy. Lactose intolerance is an uncommon diagnosis below the age of three years and cow’s milk allergy is a more likely diagnosis.
Delays in diagnosis of CMA are recognised with the study by Sladkevicius stating an average of 3.6 months to diagnosis.4 This negatively impacts on quality of life for effected families and can generate unnecessary costs in prescribing, primary care consultations and hospital attendances.4
The last five years has seen publications of NICE guidance on diagnosis of food allergy2 and for milk allergy management in the UK, NICE Clinical Knowledge Summary,5 MAP (Milk Allergy in Primary Care)6 and BSACI (British Society of Allergy and Clinical Immunology) guidelines.1
2016 also saw the publication of the NICE Quality Standard on Food Allergy.3 It is hoped that the guidance will improve the recognition and management of infants with suspected milk allergy.
- Dr Joanne Walsh is a GP and chair of the Primary Care Group of the British Society for Allergy and Clinical Immunology (BSACI)
References
- Luyt D, Ball H, Makwana N et al. BSACI guideline for the diagnosis and management of cows’ milk allergy. Clin Exp Allergy 2014; 44(5): 642-72.
- NICE Guidance CG116. Food allergy in under 19s: assessment and diagnosis. February 2011
- NICE Quality Standard QS118. Food allergy. March 2016.
- Sladkevicius E, Nagy E, Lack G, Guest JF. Resource implications and budget impact of managing cows’ milk allergy in the UK. J Med Econ 2010; 13(1): 119-128
- NICE Clinical Knowlege Summaries. Cows’ milk protein allergy in children. Last revised June 2015.
- Venter C, Brown T, Shah N, Walsh J, Fox AT. Diagnosis and management of non-IgE-mediated cows’ milk allergy in infancy – a UK primary care practical guide. Clin Transl Allergy 2013; 3:23.