While most people are aware of the link between smoking and cancer, 3 in 4 are unaware that being overweight (BMI between 25 and 29.9) or obese (BMI of 30 or more) is the second biggest preventable cause of cancer.1
The evidence linking bodyweight and cancer has been building for decades, with new evidence still emerging.
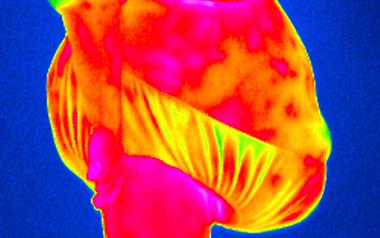
Excess bodyweight linked to 13 types of cancer
As with smoking, carrying too much weight doesn’t just affect one type of cancer. There’s now strong evidence that shows carrying too much weight increases the risk of 13 types of cancer.2
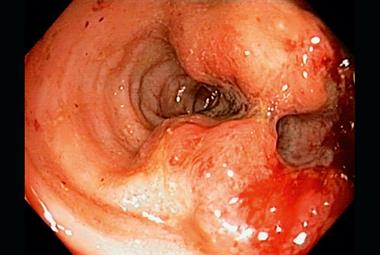
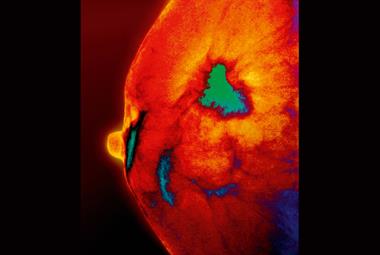
This includes some of the most common, such as breast and bowel cancers, but also some of the hardest to treat, such as oesophageal cancer.
And the effect is particularly strong in womb cancer.3 Studies have shown that obese women have more than twice the risk of developing womb cancer compared to women who are a healthy weight.2
 Cancer Research UK
Cancer Research UKFor more like this, sign up to
Cancer Insight for GPs.
Cancer Insight is your free guide to cancer prevention and early diagnosis from Cancer Research UK.
This article has been funded by Cancer Research UK for GP Connect
How does weight affect cancer risk?
Researchers are still trying to determine exactly how carrying extra weight causes cells to become cancerous. But it’s likely to be down to the hormones and other growth-promoting signals released from the extra body fat, also causing inflammation. Each of these affects cell division and are most likely behind the increased risk of cancer.
Why health professionals need to tackle obesity right now
Around 60% of adults and 30% of children in the UK are overweight or obese and this trend is set to continue unless we act now.
Reducing the prevalence by just 1% each year could avoid 64,200 cases of cancer over the next 20 years and save around £40 million in NHS costs annually from 2035.
How GPs can encourage weight loss in just 30 seconds
Well-established in smoking cessation counselling, new research, part funded by Cancer Research UK, shows very brief advice is also an effective and acceptable intervention for tackling obesity.
While many GPs are nervous about discussing weight and potentially damaging relationships with patients, the study, published in The Lancet, found that 8 in 10 patients felt the very brief conversation with their GP about weight was both appropriate and helpful.4
It took just 30 seconds for the GPs involved in the trial to deliver very brief advice about weight, which was based around the following framework:
- ASK patients if they would like to talk about their weight, respecting their decision if they choose not to. (Recording a patient’s weight can help to open up conversations.)
- ADVISE on what support is available in the practice and local area.
- ACT by referring patients on to available support schemes, such as Slimming World, free on the NHS.
Weight loss results following the intervention were encouraging showing that even a short conversation between a GP and a patient about losing weight can be extremely effective.
- Dr Richard Roope is RCGP and Cancer Research UK Clinical Champion for Cancer, and Cancer Research UK Senior Clinical Advisor.
References
- Cancer Research UK. Public knowledge of the link between obesity and cancer. 2016.
- Lauby-Secretan, B. et al. Body Fatness and Cancer — Viewpoint of the IARC Working Group. N Engl J Med 2016; 375: 794-8. 2
- Zhang, Y. et al. Overweight, obesity and endometrial cancer risk: results from a systematic review and meta-analysis. Int J Biol Markers. 2014; 29(1): e21-9.
- Aveyard, P. et al. Screening and brief intervention for obesity in primary care: a parallel, two-arm, randomised trial. Lancet 2016; 388: 2,492-2,500.